I don’t know. I learned all of this over the course of 3 months. Now I sit here, far down the road from where I began with a wealth of information. Information I wish I had more readily organized and made available to me. Man, that would have really helped me from the start.
The challenging thing with pain is that it's such a subjective experience. It's difficult to find where it actually hurts. It's difficult to describe the feeling. Sometimes what we call pain is a building, nagging discomfort, and other times it's an acute pain. The pain also can shift, and move and change locations, making it hard to pinpoint. And this can play games with our own mind.
For me things presented initially with that age-old “crick” in the neck. That stiff neck that hurts when you turn to one side or another, but after a few days it goes away. Only this time, it didn’t go away, and it grew and morphed into all sorts of new pains I'd never had before. And it was all at once and everywhere.
At this point, i wasn’t sure where to turn. So I went where most of us would go first. I went to my Primary Care Provider (PCP) first. I’m sure he hears from a wide range of complainants. From the worried well, to the acutely ill, and to those who are just seeking drugs and attention. I’m not any of the above. I hate going to seek care. I hate being on medicine. We have a 14 year relationships my PCP and I. So you’d think he’d take all of this into consideration. I after all was in enough discomfort to come and see him.
His first course of action was to push me to rest, take ibuprofen, do some physical therapy (PT) or massage. He was insistent, it was just some muscle spasms or knots and that it would go away. While I heard him, this pain was different. His reaction left me feeling a bit gaslit and I began to second guess myself. Maybe I was just being a wuss. I left, had a very painful, pointless massage, and messaged him again a few days later.
“I’m in excruciating pain! ”
“Suck it up, buttercup”
Defining the Symptoms
This is the hardest part to describe, and I’ll probably remember more over time. The symptoms at the core were roughly the same, but also constantly changed. I even asked ChatGPT to visualize my pain at one point!
Dall-E doing its best to visualize my pain
Instead of a long description, I’m just going to list all the ways I was feeling pain.
Neck pain that felt like electric ropes, on both sides of my neck, and into the front bundle of nerves near my clavicle. These would hurt to touch and on any movement of the neck that used the muscles or touched those nerves.
That turned into pain, both feelings of muscle tightness, soreness and cramping in my upper traps, and sometimes mid traps. On the left side in particular it would increase with such intensity, any bending at the hip or up and down (vertical to the ground) movements would cause intense pain.
It would eventually calm down with ibuprofen, but if I ever went for a walk, within 20 minutes the pain would return. My best day of walking day, I was able to manage a 60 minute walk, but to my surprise, I walked less than a 2 mile per hour pace.
I felt what can only be described as a needle piercing my shoulder joint from time to time. Just for a little extra fun, it would throb, almost burn at times as well.
Most of my pain was originally concentrated on the left side of my body. You can imagine how demoralizing it was when one day it began to migrate and coexist on the right side as well (though less severely).
I had one final very painful symptom, which was a distressing feeling in my cervical spine (I might have called it my neck. The part of your neck you reach back and hold behind your head). This would make me shudder with pain in a variety of situations. I learned later that this was a pretty dead giveaway that I had some kind of disc problem. The pain would appear when..
I sat on the toilet.
On the release of the sphincter when on the toilet*
When I got up off the toilet (the bending part, I started squatting to get up and down from then on)
Coughing
Sneezing
Sometimes Just talking, when I projected my voice
Sometimes on the top of an exhale, transitioning to an inhale
There were times that I felt like, can’t anyone else grasp how much pain I am in? How is the world still functioning? How am I still existing? Am I a wuss? My doctor’s responses to me certainly had me continuing to feel like a complainer. I was so lost, i even wrote a poem to describe my pain.
These symptoms are tricky to track to the source. But when you peel back the onion, you know that these are all interrelated, connected, and are often referring from another original source. And they are awful. After a ton of different searches, I had found this thread on Reddit that gave me some validity to my pain and the likely term that described it, radiculopathy.
Initial Symptom Treatment
As I’ve described, my primary care provider was minimally involved and rather dismissive of my pain. As I thought about my journey here, I also realized that the PCP is not well suited to helping one manage their pain. They diagnose, prescribe, or refer to specialists. They do not manage chronic conditions and definitely don’t really help with musculoskeletal issues.
So I went to a chiropractor. Not for the cracking of bones, but because I had a referral from a good friend. She had used the same guy for other ailments, and she felt he was a sports oriented practitioner and really listed to her. He was a guy who would work on helping me stretch things out. If my condition was simply inflammation and muscle spasms as my PCP suggested, then the pain was just trying to protect me from something strained. Sometimes its thought the mind needs some reminding at some point that its ok to let go. You know, “go to the pain.” At some point my mind could be shown through stretch work that its ok to start the normal movements again. Sort of a retraining of your brain so that the neural pathways can “let go” (these are my words to keep things simple).
This stretch work gave me some relief after a few weeks. At this point ibuprofen was starting to have some positive impact. This gave me a little bit of hope that I was improving. My PCP still avoided any more rigorous meds. In spite of some of this progress, I was still unable to walk more than 20 minutes at a 2 mph pace before turning around in pain.
Now, a new symptom emerged. I was starting to feel some tingling in my arms, and occasional numbness in my hand. This progressed quickly. Next I was beginning to feel like my left hand didn’t quite have the same motor control as my right hand. I’d say it was 95% of the other hand. That soon moved to my bicep. If I carried a stack of plates from the dishwasher to put away, my left hand would slowly start falling with the same stack of plates as my right hand. This was more concerning and a new set of symptoms. It's what I would learn was a condition called Myelopathy.
Before he worked on my body, my chiropractor ordered an X-Ray. My neck and vertebrae all looked healthy, well aligned and in good shape. Since a few weeks of treatment didn’t improve things and I developed new symptoms that diminished motor control and strength, again my chiropractor ordered an MRI. I had seen my PCP again in between, and his recommendation was to stay the course. Do nothing. Luckily for me, I had that MRI done. The results were startling.
The MRI found the smoking gun
The MRI showed I had severe spinal stenosis between C3 and C4 in my neck. That is, my disc had exploded and was putting a ton of pressure on my spinal cord, pinching it severely. The exploding disc (my words) is called a disc extrusion. The nucleus of the disc had burst out from the middle and through of the outer layer. It was oozing into my spinal cord (this is my version of the clinical description). My chiropractor sent it to a neurosurgeon colleague of his who was shocked that I was walking and not already paralyzed!
My entire world was flipped upside down over the next 10 days. It turns out that when you have a disc bulging, or the nucleus bursts from the inside of the disc and leaks out, it can put pressure on the nerve bundles in that spinal segment or on the spinal cord itself, this is known as spinal stenosis. In my case, I had a severe case of it.
The symptoms I was now experiencing had a root cause. The disc extrusion, and the subsequent spinal stenosis. They also had names.
When the disc extrusion puts pressure on the nerve bundles, the result can be a condition known as Radiculopathy, or Cervical (neck) Radiculopathy. This was the cause of my pain. This was not just an inflammatory response or muscle spasms from a muscle strain or knot. This was my body saying, “woah, we have problems here, you need to shut down and rest until I can heal this.”
When it puts pressure on the spinal cord, you can have a totally different set of symptoms. Given how high up my spine my issues were (C3 - C4 is just below the base of your skull), all the nerves coming from my brain to control my entire body have to pass through that segment. Which means pressure to that point can affect my entire body function, and can present anywhere. The common impact is tingling, numbness and then loss of strength and motor control. This condition is called Cervical (neck) Myelopathy. As I learned more about this condition, I learned that it is often irreversible. Once you’ve done the damage, it often does not come back to full function. So as your condition progresses you have interventional decisions to make before things get too bad.
Cervical Radiculopathy vs. Cervical Myelopathy in a Spinal Stenosis Condition
Dr. Brian Su, Orthopedic Surgeon Marin Health: Cervical Stenosis, Spinal Cord Compression and Myelopathy. DO I REALLY NEED SURGERY?
After learning all about these conditions and visiting with the neurosurgeon, I stopped all work on the neck. I am fortunate, having worked in healthcare for 20 years to have a decent network of physicians of all specialties in my network. I shared my images with as many doctors as I could. Including my own PCP. Every doctor I shared it with general PCPs, and specialists generally had the same reaction. Their faces would go white, they would say, “I’m so sorry,” “don’t move that neck” and then start suggesting various interventions. Usually they suggested a Spinal Fusion.
My Cervical Spine MRI
A Healthy Cervical Spine MRI
In case its unclear, the column down the middle of the image is the spinal cord. The white stuff on each side is spinal fluid. It should be clean like on the right, but mine was getting pushed in as you can see and you can even see some of the nucleus dripping down between the two segments C4 & C5.
Decisions to Make
Over the next week, I became a sponge, collecting much of the information you see here. Before I understood what Myelopathy was, I even though maybe my body could heal this itself. I now fully understood how the various diagnoses from the MRI drove the symptoms, both the Radiculopathy (pain) and the Myelopathy (numbness, tingling & weakness).
Cervical Sections and Disc Areas and how they radiate pain with Radiculopathy
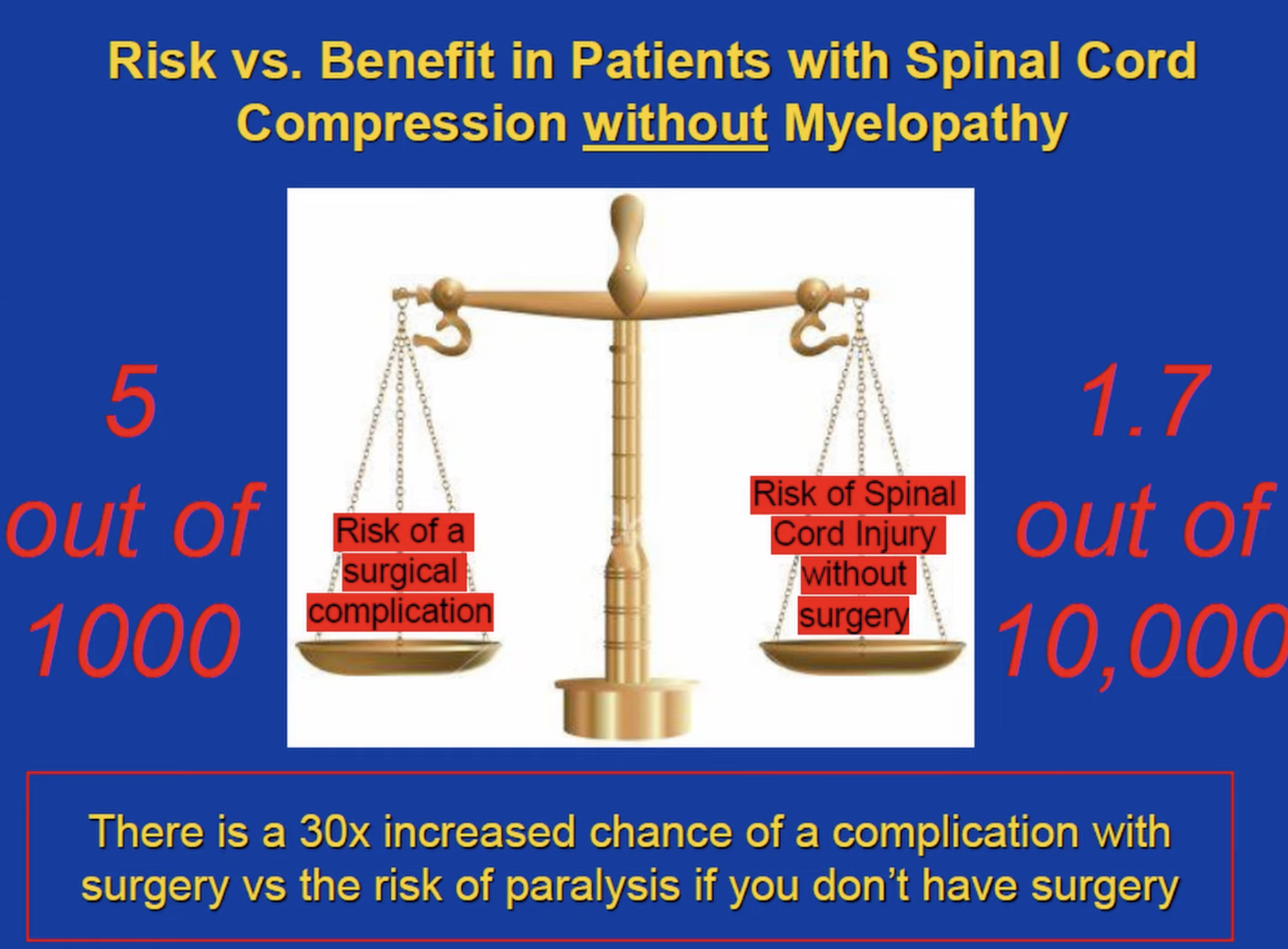
Spinal Cord Risk without Myelopathy Present vs. Surgical Risk
There are a lot of charts like the above, this one with its primary & secondary were more full descriptions. My chiropractor assumed I might have issues between C5 & C6 based on my symptom descriptions.
I now began wondering about the risks of surgery vs. not doing surgery. Surgery comes with its own inherent set of risks. Both during and after. Any procedures I would have to undergo would require intubation and anesthesia, and complications during surgery or the risk of infection at the place where surgery would happen were among the many possible negative outcomes. I had also just been warned that there was a risk of paralysis just living my life day to day. I found a video from Dr. Brian Su, an orthopedic spine surgeon at Marin health that did an outstanding job of breaking down the options, probabilities and when to do surgery or not. I’ve linked to it below and pulled a few stills from his video.
Dr. Brian Su, Orthopedic Surgeon Marin Health: Cervical Stenosis, Spinal Cord Compression and Myelopathy. DO I REALLY NEED SURGERY?
He also pointed to a lot of work by the Japanese on the subject of Myelopathy in particular, including a survey used to measure severity of symptoms. It's called the mJOA score. You can see the basic set of questions below, and give yourself a score.
mJOA Severity Questionnaire/Assessment for Myelopathy
A few days after my neurosurgeon visit, I began noticing tingling down my left leg from my hip and groin all the way to my foot. This was clearly a new set of symptoms and starting to show progression. The thing that pushed me towards accelerating surgery was a similar loss of motor control in my foot. I twice stumbled as my left leg was not moving as fast as my right leg, and particularly my foot, would not always complete a step. It almost felt like my right leg was in 5th gear, while my left leg was in 4th gear. The next potential list of progressive symptoms included loss of bladder and bowel control. It was then that I realized that the consequences of inaction were severe.
The compounding factor if you listen to Brian Su’s video is that Myelopathy is often irreversible. The procedures that are done on the neck are intended to stop progression and not done to reverse symptoms.
I found another great visual from Dr. Sheyan Armahani that shows how quickly the progression can happen and the little false senses of improvement you can feel before another jump in disability.
Will you ever get better? Myelopathy Progression Graph
Dr. Sheyan Armeghani, Orthopedic Surgeon Orlando Health: Cervical Myelopathy - What is it? How can we treat it?
With my own progression, it was no longer a question of should I treat the symptoms with surgery, or when should I schedule it. It was now about which surgery should I do and how soon could I do it.
Spinal Fusion or Disc Replacement
In my case I had a very clean set of discs and vertebrae, other than the problem spot. Spinal fusion and Artificial Disc replacements were the two most common procedures done for my condition. Spinal fusion has been around since the 1950s and has a lot of data behind the outcomes and it's what most spine and neuro surgeons tend to do. Disc replacements have been around since the early 2000s so there is no one alive who’s really had one for more than 25 years. This is becoming more mainstream but it's tough to find a surgeon who will do them and has done a lot of them. If I learn of a better way to find this, I'll publish it. But as of now, I know of no sources that the general public has to search for surgeons who perform a specific surgery and have a high number of procedures and positive outcomes.
I found a good set of overviews from Dr. Dan Lieberman from the Phoenix Spine Institute who tried to break down some of the data from a few NIH studies on both procedures. Link to that video here. As with all data and analytics, I found every study I read to be missing something, or misleading. You’d hear that there was significant ASD (adjacent segment degeneration) of the vertebrae above or below where you had a Spinal Fusion procedure after 10 years. But if you kept digging, you’d see that the percentage listed was just that it was discovered in the MRI, and only ½ that number were symptomatic and even smaller percentage required intervention.
The stat that Dr. Lieberman pulled out that stood out most to me was this one.
Satisfaction With Surgery
Journal of Neurosurgery: Cervical disc arthroplasty: 10-year outcomes of the Prestige LP cervical disc at a single level
There is plenty of data that both Spinal Fusion and Total Disc Replacements both have high success rates post surgery. This study states that there’s a high satisfaction rate with both procedures as well, with a slight edge to the Total Disc Replacement. Longer term studies, taken after 10 years also suggest good outcomes for both procedures.
My final decision was based on the fact that I’m young and healthy, deemed a good candidate based on my imaging work, I had a great surgeon who had done many disc replacements, and that it had the fastest recovery time and best range of motion long term. There were some further studies that indicated that there was less adjacent segment degeneration from the disc replacement (which makes sense as the neck has full range of motion). Maybe the last thought I had was well, if the disc replacement fails at some point, spinal fusion will always be a backup option. If the Spinal Fusion fails, what’s my real fallback?
Again, i’m sharing my journey, you’ll have to find your own logic, do as much research as you can and interpret the findings. These things are highly personal and everyone has their own level of risk tolerance. The one thing I can give some guidance on is your internet search. I’ve found that overwhelmingly most posts you’ll find in discussion threads and on Reddit will be from people who have had a negative experience. It was at first quite alarming, but also I realized at odds with the high success rates quoted in most of the studies. There is definitely a bias towards posting about negative experiences. Same can be said when speaking with physical therapists. Many of their patients all into the unsuccessful surgery category.
Total Disc Replacement and Post Procedure
As you can probably guess by now, I opted for the Total Disc replacement. My surgeon recommended the Prodisc C, made by a company called Centinel Spine. Turns out the device manufacturers put out a LOT of information about the procedure including the statistics (of course from their perspective).
This video by Centinel Spine does a great job showing you exactly what the procedure was and I’ll link to their website which also has a ton of information. If I had to do it over, i might actually start here as they have some of the best put together information. Its their job after all to convince you to give their procedure a go!
I’ve built and posted this content 2 weeks post procedure. I am grateful for the chance to have this surgery, and for the surgery itself to have been successful. My primary recovery focus was actually on the surgical wound. The procedure requires an incision in the neck and moving your esophagus and other parts aside to give space to replace the disc. That area was swollen, and caused the greatest discomfort. The nerves under my chin are also disrupted, and I’m numb there. My surgeon indicated this may take 8 months to improve.
So far, i have seen a significant reduction in Radiculopathy, and in the Myelopathy too. There is still numbness in my foot and in other areas at times. I am going to be careful until all of that feeling returns and I hopefully regain strength in the areas I lost. I am grateful for the procedure, as I think it saved my life and I’m very optimistic about recovering and getting back to who I was before the pain began. I’ll post more about my post procedure journey here after its been some time.